There are four types of PCOS: Insulin-resistant PCOS, Inflammatory PCOS, Adrenal PCOS, and Pill-induced PCOS.
- Insulin-resistant PCOS: This type arises when the body struggles to use insulin effectively, often leading to an increased risk of type 2 diabetes.
- Inflammatory PCOS: Triggered by chronic inflammation, this type can exacerbate hormonal imbalances and worsen PCOS symptoms.
- Adrenal PCOS: Often elusive, this type is characterised by underlying factors that aren’t immediately apparent but can significantly impact hormonal health.
- Pill-induced PCOS: Resulting from the discontinuation of certain birth control pills, this type can mimic PCOS symptoms and often resolves over time.
Table of Contents
What is PCOS? An Introduction to this Complex Hormonal Disorder
PCOS, or Polycystic Ovarian Syndrome, is a hormonal disorder characterised by:
- Irregular menstrual cycles
- Elevated levels of androgens
- And often, the presence of multiple small cysts on the ovaries
Many women are affected by PCOS, impacting their hormonal balance, menstrual cycles, fertility, and overall health.
If you have been diagnosed with PCOS, you will find the information below invaluable in understanding the nuances of your condition and empowering you to take informed steps towards better health. Gaining insight into the various types of PCOS is a crucial step in this journey.
In my experience, you can get PCOS under control with a few lifestyle changes, including regular exercise and a healthy diet.
Have You Been Diagnosed with PCOS?
If you’ve received a PCOS diagnosis, you might have ventured down various treatment paths, only to find they didn’t quite resonate. You’re not alone in this journey, and it’s not uncommon to feel that the standard approach to PCOS management isn’t tailored to your unique needs.
This feeling often arises because PCOS is not a one-size-fits-all condition. It is intricate, multifaceted, and deeply personal. While doctors may often identify the dominant type of PCOS, there’s so much more beneath that primary diagnosis, waiting to be understood and addressed.
In fact, subdominant types, often lurking in the shadows, can play a pivotal role in how you experience this condition. Recognising and addressing these can be transformative, guiding you towards a treatment that feels right for you.
In this article, we’ll explore the different types of PCOS, highlighting the often-overlooked types that might influence your journey. With this knowledge, you’ll be better positioned to find a treatment approach that truly resonates with you.
Remember, every individual’s experience with PCOS is unique, and understanding yours is the key to better management.
A Deeper Look into PCOS: Beyond Ovarian Cysts
Polycystic Ovarian Syndrome (PCOS) is not a singular disease but a collection of symptoms stemming from various underlying factors. PCOS shows up in many ways; you may see these signs:
- Missed or late periods often happen
- Hair grows where it doesn’t usually, like on your face or belly
- Skin spots called acne can cover your face and body
- Putting on a lot of weight can happen very fast
- Although you try, getting pregnant is tough
- You feel tired all the time without reason
- Dark skin spots appear on the back of your neck or under your arms
While the name might suggest a primary focus on ovarian cysts, it’s crucial to understand that they are just one aspect of the condition.
The presence of cysts is not always a definitive diagnostic criterion. More central to PCOS are hormonal imbalances, particularly elevated androgen levels, which can significantly impact an individual’s health and well-being.
The 4 Types of PCOS
It is very hard to know which type of PCOS you have unless tests are carried out. Also, you likely have more than one type of PCOS.
This complexity often requires a combination of hormonal, metabolic, and ultrasound assessments to pinpoint. Understanding the full spectrum of your PCOS types can provide clarity and guide more effective treatment strategies.
The table below clearly defines the symptoms associated with each type of PCOS. It’s important to note that while these symptoms can indicate a specific type of PCOS, they can also overlap, and a comprehensive assessment by a healthcare professional is essential for an accurate diagnosis. Following the table, we delve deeper into each type of PCOS, providing a more detailed understanding of their unique characteristics and implications.
The Four Types of PCOS: Comparative Symptoms
| PCOS Types/Symptoms | Insulin Resistance PCOS | Adrenal PCOS | Inflammatory PCOS | Post-Pill PCOS |
|---|---|---|---|---|
| Irregular Menstrual Cycles | Yes | Yes | Yes | Yes |
| Weight Gain/Issues | Yes (especially around waist) | No | No | Possible |
| Excessive Hair Growth | Yes | Mild | No | Temporary |
| Acne/Oily Skin | Yes (jawline/chin) | Yes (jawline/chin) | Yes | Temporary |
| Scalp Hair Thinning | Yes | Yes | No | Temporary |
| Elevated DHEA-S Levels | No | Yes | No | No |
| Absence of Insulin Resistance | No | Yes | Yes | Yes |
| Chronic Fatigue | No | No | Yes | No |
| Joint Pain | No | No | Yes | No |
| Digestive Problems | No | No | Yes | No |
| Mood Fluctuations | No | Yes | Yes | Yes |
| Ovarian Cysts | Possible | No | No | Temporary |
| Sensitivity to Foods | No | No | Yes | No |
| Breast Tenderness | No | No | No | Yes |
Let’s look at each type of PCOS in more depth.
1. Insulin Resistance PCOS
Insulin Resistance PCOS arises when your body produces insulin but struggles to use it efficiently. This inefficiency poses a significant concern, as it heightens the risk of progressing to type 2 diabetes.
By adopting certain lifestyle changes, those with Insulin Resistance PCOS can potentially lower their chances of developing type 2 diabetes.
It’s worth noting that this form of PCOS is not only the most prevalent but also among the most concerning due to its associated health risks.
Insulin Resistance PCOS: A Closer Look
When dealing with Insulin Resistance PCOS, it’s crucial to be aware of the heightened risk of developing type 2 diabetes. But here’s a key insight: for an accurate diagnosis, the hormone insulin should be measured, not just glucose. This distinction can make all the difference in understanding and managing the condition. On the treatment front, supplements like magnesium and inositol have shown promise in offering relief and balancing insulin levels.
What are the symptoms?
- Irregular Menstrual Cycles: Periods that are infrequent, irregular, or even absent.
- Weight Gain: Especially around the waist.
- Difficulty Losing Weight: Even with diet and exercise.
- Fatigue: Feeling constantly tired or lacking energy.
- Darkened Skin Patches: Often found on the neck, elbows, knees, knuckles, and armpits.
- Skin Tags: Small, painless growths on the skin.
- Acne: Particularly along the jawline and chin.
- Excessive Hair Growth: Especially on the face, chest, and back.
- Thinning Hair or Hair Loss: On the scalp.
- Cravings: Particularly for sugary or carbohydrate-rich foods.
It’s important to note that while these symptoms can be indicative of Insulin Resistance PCOS, they can also be associated with other conditions. It’s always best to consult with a healthcare professional for a proper diagnosis.
How exercise can help
Exercise can help to reduce insulin resistance PCOS. Regular exercise as well as moving throughout your day can really help you to build muscle and burn calories. Most interestingly, it can improve your sensitivity to insulin. Low insulin sensitivity is the problem behind insulin resistance PCOS!
2. Adrenal PCOS
Adrenal PCOS occurs when the ovaries produce excess androgen, which can lead to adrenal dysfunction. This dysfunction can further exacerbate hormonal imbalances, leading to a cycle of increased androgen production and adrenal stress.
Adrenal PCOS: Understanding the Connection
Adrenal PCOS often gets mistaken for or overlaps with a genetic condition known as late-onset congenital adrenal hyperplasia (CAH). It’s essential to recognize this similarity as it can guide diagnosis and treatment. Speaking of treatments, there are several natural remedies that can be beneficial. Consider incorporating supplements and herbs like magnesium, zinc, licorice, adaptogen herbs, and pantothenic acid (also known as vitamin B5) to help manage and alleviate symptoms.
What are the symptoms?
- Irregular Menstrual Cycles: Periods that may be infrequent or absent.
- Mild Hirsutism: Excessive hair growth, especially on the face, chest, and back.
- Acne and Oily Skin: Particularly along the jawline and chin.
- Scalp Hair Thinning: Noticeable hair loss or thinning on the head.
- Elevated DHEA-S Levels: Higher levels of the adrenal androgen DHEA-S in blood tests.
- Normal LH and FSH Ratios: Unlike other types of PCOS, these hormones’ ratios often remain normal.
- Absence of Insulin Resistance: Typically, no signs of insulin resistance are present.
- Mood Fluctuations: Increased feelings of anxiety or mood swings.
- Fatigue: Feeling constantly tired or lacking energy.
As with any PCOS, it’s essential to consult a healthcare professional for an accurate diagnosis, as these symptoms can overlap with other conditions.
How exercise can help
Exercise can help to reduce adrenal dysfunction PCOS. Regular exercise and movement throughout the day help reduce stress, which may help restore adrenal function.
3. Inflammatory PCOS
Inflammatory PCOS arises due to chronic inflammation, which can disrupt hormonal balance and exacerbate PCOS symptoms, creating a cycle where inflammation feeds the disorder and vice versa.
Inflammatory PCOS Causes
Inflammatory PCOS isn’t just a name; it points to underlying inflammation that can exacerbate the condition. But what causes this inflammation? It can stem from various sources, including food sensitivities that might be triggering unwanted reactions, gut issues that disrupt the body’s natural balance, or even chronic mast cell activation, a lesser-known but impactful factor. To help combat this inflammation and its effects, consider adding supplements to your regimen. Both zinc and N-acetyl cysteine have shown promise in offering relief and reducing inflammation associated with this type of PCOS.
What are the symptoms?
- Irregular Menstrual Cycles: Infrequent, irregular, or even absent periods.
- Chronic Fatigue: Persistent feelings of tiredness or lack of energy.
- Joint Pain: Discomfort or aches in the joints without apparent injury.
- Skin Issues: Conditions like acne, rosacea, or skin redness.
- Digestive Problems: Including bloating, stomach pain, or irritable bowel syndrome (IBS).
- Sensitivity to Certain Foods: Reactions or intolerances often lead to digestive issues.
- Chronic Headaches or Migraines: Persistent or recurring headaches.
- Mood Disorders: Including depression or mood swings.
- Recurring Infections: Frequent illnesses or infections due to a potentially weakened immune system.
It’s crucial to remember that while these symptoms can indicate Inflammatory PCOS, they can also be associated with other conditions. Consulting with a healthcare professional for a proper diagnosis is always recommended.
How exercise can help
Exercise can help to reduce inflammation PCOS. Regular exercise and movement throughout the day help improve joint pain, reduce headaches and help with fatigue, all symptoms of inflammation PCOS.
4. Post-Pill PCOS
Although not considered “real” PCOS, post-pill PCOS can still affect ovulation and mimic many of the symptoms associated with traditional PCOS, especially in the months immediately following the discontinuation of birth control.
Post-Pill PCOS: A Transitional Phase
If you’ve recently stopped taking certain birth control pills and are experiencing PCOS-like symptoms, you might be dealing with Post-Pill PCOS. It’s important to note that this is often a temporary condition. While it can be concerning to face these symptoms suddenly, there’s a silver lining: many individuals find that Post-Pill PCOS resolves on its own over time. It’s a reminder that our bodies can go through transitional phases, especially after changes in hormonal treatments.
What are the symptoms?
- Irregular Menstrual Cycles: Delayed periods or amenorrhea (absence of periods) after stopping birth control pills.
- Temporary Androgen Excess: Symptoms like acne, hair thinning, or hirsutism (excessive hair growth).
- Ovarian Cysts: The presence of multiple small cysts on the ovaries, often detected through ultrasound.
- Mood Fluctuations: Mood swings, anxiety, or depression after discontinuing the pill.
- Breast Tenderness: Sensitivity or pain in the breasts.
- Weight Changes: Weight gain or difficulty losing weight.
- Ovulatory Issues: Difficulty in tracking ovulation or anovulatory cycles.
- Spotting Between Periods: Light bleeding or spotting between regular menstrual cycles.
It’s important to note that these symptoms are often temporary and may resolve independently as the body adjusts post-pill. However, it’s always a good idea to consult with a healthcare professional if symptoms persist or are of concern.
How exercise can help
Exercise can help to reduce your risk of developing post-pill PCOS. Post-pill PCOS can go away by itself after 3-6 months but regular exercise and lifestyle changes can help you to get rid of it even quicker.
Clarifications: Polycystic Ovaries vs. Androgen Excess
Navigating the world of PCOS can sometimes be a maze of terms and conditions. Let’s clear up a few things:
Polycystic Ovaries vs. Androgen Excess
Having polycystic ovaries doesn’t necessarily mean you have PCOS. It’s possible to have multiple cysts on the ovaries without the hormonal imbalances typical of PCOS. On the flip side, the hormonal condition of androgen excess is a defining feature of PCOS, even if cysts aren’t present.
Other Causes of Androgen Excess
While PCOS is a common cause of increased androgens, it’s not the only one. Conditions like congenital adrenal hyperplasia can mimic PCOS symptoms. Elevated prolactin levels, often due to issues with the pituitary gland, can also lead to androgen excess. Some hormonal birth controls with a high androgen index can also trigger similar symptoms.
Understanding these nuances can help get a clearer picture of your health and ensure you’re on the right path to management and recovery.
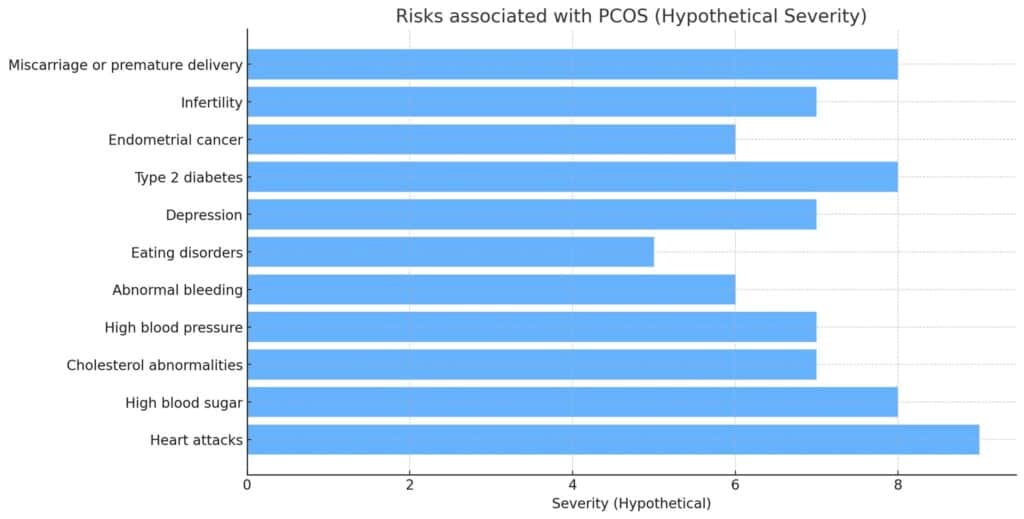
Risks Associated with Each Type of PCOS
About PCOS Diagnosis
When it comes to diagnosing PCOS, it’s not always a straightforward journey. Here are some key points to keep in mind:
Ruling Out Other Conditions
Before landing on a PCOS diagnosis, it’s crucial to rule out other conditions that might present similar symptoms. This ensures that you’re treating surface-level symptoms and addressing the root cause.
Criteria for Diagnosing PCOS
A PCOS diagnosis typically relies on a combination of factors, including irregular menstrual cycles, signs of androgen excess, and polycystic ovaries in ultrasounds. However, remember that having cysts alone doesn’t confirm PCOS.
Pain and PCOS
While many symptoms are associated with PCOS, pain isn’t typically one of them. If you’re experiencing pain, especially severe or chronic, it’s essential to consult with a healthcare professional to explore other potential causes.
PCOS vs. Hypothalamic Amenorrhea
These two conditions can sometimes be confused due to overlapping symptoms like missed periods. However, hypothalamic amenorrhea is often caused by stress, extreme weight loss, or excessive exercise and lacks the androgen excess seen in PCOS.
Gaining a clear understanding of the diagnosis process and differentiating between similar conditions can be empowering, ensuring you’re on the right path to effective management.
PCOS Treatment
Navigating PCOS treatment can feel overwhelming, but understanding your unique needs can make all the difference. Here’s what to consider:
Personalised Treatment
PCOS isn’t a one-size-fits-all condition. Each type of PCOS has its own challenges and requires a tailored approach. By understanding your specific type, you can work with your healthcare provider to develop a treatment plan that truly resonates with your body’s needs.
Cyclic Progesterone Therapy
One of the promising treatments for PCOS is cyclic progesterone therapy. It acts as a natural anti-androgen treatment, helping to balance out elevated androgen levels often seen in PCOS. This therapy can especially benefit those seeking a more natural approach to managing their symptoms.
Remember, the journey to managing PCOS is deeply personal. By advocating for treatments that align with your specific type and needs, you’re taking a proactive step towards better health and well-being.
Addressing PCOS Through Holistic Nutrition and Support
While we’ve delved into the types of PCOS, it’s crucial to understand that treating PCOS is not a one-size-fits-all approach. The types of PCOS include variations due to factors like abnormal blood sugar levels, a surge in androgens, or issues with the adrenal glands and nervous system.
A nutritionist can play a pivotal role in crafting a diet that supports the adrenal glands, balances blood sugar, and promotes gut health. For instance, incorporating natural anti-inflammatories such as turmeric can help reduce inflammation. Nutrients like magnesium in supplements can support the pancreas and help cells become more responsive to insulin, curbing those persistent sugar cravings. Omega 3 fatty acids, vitamin E, B6, and antioxidants like NAC are also beneficial.
Unexplained fatigue, skin issues like eczema, and facial hair growth (a result of male hormones like excess androgens) can be distressing. These symptoms might be linked to factors such as an imbalance in the follicle-stimulating hormone or a rise in C-reactive protein. Consider magnesium, chromium, vitamin B5, and vitamin C supplements to address these. They not only support the adrenal glands but also aid in repairing leaky gut tissue and balancing gut bacteria. Improving digestive enzymes is another step towards holistic health.
Avoid high-sugar diets and focus on foods rich in antioxidants. Medications like spironolactone or natural remedies like peony can also be considered, but always under professional guidance.
Find below examples of some steps you can take:
- Eat a balanced diet with plenty of fruits, vegetables, whole grains, and lean proteins.
- Incorporate foods that help regulate blood sugar levels, such as complex carbohydrates and fibre-rich foods.
- Limit your intake of processed foods, sugary snacks, and drinks high in added sugars.
- Engage in regular physical activity to help manage weight and improve insulin sensitivity.
- Aim for at least 150 minutes of moderate-intensity exercise each week.
- Practice stress-management techniques like meditation or deep breathing exercises.
- Get enough sleep to support hormonal balance and overall well-being.
- Consider creating a personalised nutrition plan with a registered dietitian or healthcare professional.
In conclusion, while each type of PCOS may require different treatments, the overarching goal remains to restore balance and well-being.
Whether through dietary changes, supplements, or stress reduction techniques, there’s a path to better health for everyone with PCOS.
The Role of a Personal Trainer in Your PCOS Journey
Navigating the intricacies of PCOS can often feel like a solitary journey, but I want you to know that you don’t have to face it alone. As a personal trainer, I’ve seen firsthand how tailored fitness and support can transform the PCOS experience (please visit my PCOS personal trainer page and my dedicated PCOS page for more information).
Here’s why I believe this approach can make a difference:
1. Tailored Workouts for Your PCOS Type
PCOS is as unique as you are. I’m committed to understanding your specific type of PCOS and crafting workouts that resonate with your body’s needs. As PCOS isn’t a one-size-fits-all condition, neither should your fitness regimen. I will design workouts specifically tailored to your type of PCOS. For instance, exercises that improve insulin sensitivity can be emphasised if you have Insulin Resistance PCOS. On the other hand, workouts that help reduce inflammation and stress might be prioritised if you’re dealing with Inflammatory PCOS.
2. Accountability and Motivation
Having someone to guide, motivate, and hold you accountable can make a significant difference in staying consistent with your fitness goals. This consistency is crucial in managing PCOS symptoms and improving overall well-being. This is about understanding the tough days and celebrating the victories, no matter how small.
3. Holistic Approach to Health
A knowledgeable personal trainer can offer more than just exercise routines. They can provide insights into lifestyle changes, nutrition tips, and stress-reducing techniques, all of which play a role in managing PCOS.
4. Emotional Support
I understand that PCOS can be an emotional journey. Please know that you have a safe space, a listening ear, and a heart that genuinely cares about your well-being with me.
Forum Discussions on PCOS Types
As someone who’s navigated the world of PCOS professionally, I can’t stress enough the value of community. Diving into forum discussions lets you hear real stories from others just like you. Take a peek into the below forums as you might find that nugget of wisdom or that ‘aha!’ moment you’ve been searching for.
Conclusion: Taking Charge of Your PCOS Journey
Understanding PCOS is a journey, one filled with its own set of challenges and revelations.
As we’ve explored, PCOS isn’t just a singular condition but a spectrum of symptoms with various underlying causes.
From the nuances of different types to the importance of personalized treatment, it’s evident that a one-size-fits-all approach doesn’t apply here.
But here’s the empowering part: with knowledge comes the power to advocate for oneself. By diving deep into the intricacies of PCOS, you’re arming yourself with the information needed to collaborate effectively with healthcare professionals.
Remember, while this article provides a wealth of insights, consulting with healthcare experts is essential to get a proper diagnosis and a treatment plan tailored just for you.
Types of PCOS FAQs
Q: What is PCOS?
A: PCOS stands for polycystic ovary syndrome, which is a hormonal disorder that affects women of reproductive age. It is characterized by enlarged ovaries with small cysts on the outer edges.
Q: What are the symptoms of PCOS?
A: Symptoms of PCOS can vary, but common signs include irregular periods, infertility, high levels of testosterone, and excessive hair growth.
Q: How is PCOS diagnosed?
A: PCOS is typically diagnosed based on a combination of symptoms, medical history, physical examination, and various tests including hormone level analysis and ultrasounds.
Q: What causes PCOS?
A: The exact cause of PCOS is unknown, but it is believed to be related to hormonal imbalances and genetic factors. Insulin resistance and high levels of insulin also contribute to the development of PCOS.
Q: What are the different types of PCOS?
A: There are four types of PCOS: insulin-resistant PCOS, inflammation-induced PCOS, adrenal PCOS, and post-pill PCOS.
Q: What is insulin-resistant PCOS?
A: Insulin-resistant PCOS is characterized by high levels of insulin in the blood. Insulin resistance prevents the body’s cells from efficiently using insulin, leading to increased insulin production.
Q: What is inflammation-induced PCOS?
A: Inflammation-induced PCOS is caused by an imbalance in the body’s inflammatory response. Inflammatory foods and oxidative stress contribute to this type of PCOS.
Q: What is adrenal PCOS?
A: Adrenal PCOS is associated with dysfunction of the adrenal glands and the nervous system. It is characterized by high levels of adrenal androgens, such as testosterone and androstenedione.
Q: What is post-pill PCOS?
A: Post-pill PCOS refers to the development of PCOS after discontinuing the use of oral contraceptive pills. It is believed to be caused by hormonal imbalances that occur when coming off the pill.
Q: How is PCOS treated?
A: Treatment for PCOS often involves a combination of lifestyle changes, medication, and targeted therapies. Treatment options may include hormonal birth control, insulin-sensitizing medications, and natural supplements.

